Authors: Lenka Horáková, Karel Roubík
Citation
Horakova, L.; Roubik, K. Pulse Oximeter Performance during Rapid Desaturation. Sensors 2022, 22, 4236. https://doi.org/10.3390/s22114236
Fulltext in PDF & fulltext download
Published in Sensors
Download fulltext in PDF here: Pulse-Oximeter-Performance-during-Rapid-Desaturation.pdf
Download the supplementary material: sensors-1738952-supplementary.pdf
The original dataset with some other evaluated parameters (respiratory rate, heart rate) can be downsloaded here: https://ventilation.fbmi.cvut.cz/data/
NOTICE: There was a wrong image in the article published at the Sensors webpage. The error has been corrected by the publisher three days later. Nevertheless, if the article version was downloaded before its correction, here is the correct Figure 4:
Abstract
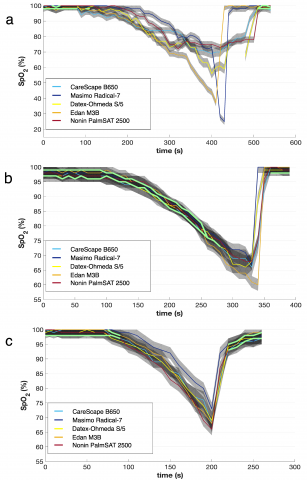
The reliability of pulse oximetry is crucial, especially in cases of rapid changes in body oxygenation. In order to evaluate the performance of pulse oximeters during rapidly developing short periods of concurrent hypoxemia and hypercapnia, 13 healthy volunteers underwent 3 breathing phases during outdoor experiments (39 phases in total), monitored simultaneously by five different pulse oximeters. A significant incongruity in values displayed by the tested pulse oximeters was observed, even when the accuracy declared by the manufacturers were considered. In 28.2% of breathing phases, the five used devices did not show any congruent values. The longest uninterrupted congruent period formed 74.4% of total recorded time. Moreover, the congruent periods were rarely observed during the critical desaturation phase of the experiment. The time difference between the moments when the first and the last pulse oximeter showed the typical study endpoint values of SpO2 85% and 75% was 32.1 ± 23.6 s and 24.7 ± 19.3 s, respectively. These results suggest that SpO2 might not be a reliable parameter as a study endpoint, or more importantly as a safety limit in outdoor experiments. In the design of future studies, more parameters and continuous clinical assessment should be included.
References
- Jensen, A.; Onyskiw, J.E.; Prasad, N. Meta-analysis of arterial oxygen saturation monitoring by pulse oximetry in adults. Heart Lung 1998, 27, 387–408.
- Dünnwald, ; Kienast, R.; Niederseer, D.; Burtscher, M. The Use of Pulse Oximetry in the Assessment of Acclimatization to High Altitude. Sensors 2021, 21, 1263.
- Griesdale, E.; Bosma, T.L.; Kurth, T.; Isac, G.; Chittock, D.R. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008, 34, 1835–1842.
- Ehrenfeld, M.; Funk, L.M.; Van Schalkwyk, J.; Merry, A.F.; Sandberg, W.S.; Gawande, A. The incidence of hypoxemia during surgery: Evidence from two institutions. Can. J. Anesth. 2010, 57, 888–897.
- De Jong, ; Rolle, A.; Molinari, N.; Paugam-Burtz, C.; Constantin, J.-M.; Lefrant, J.-Y.; Asehnoune, K.; Jung, B.; Futier, E.; Chanques, G. Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: A multicenter cohort study. Crit. Care Med. 2018, 46, 532–539.
- Baillard, ; Boubaya, M.; Statescu, E.; Collet, M.; Solis, A.; Guezennec, J.; Levy, V.; Langeron, O. Incidence and risk factors of hypoxaemia after preoxygenation at induction of anaesthesia. Br. J. Anaesth. 2019, 122, 388–394.
- Hansel, ; Solleder, I.; Gfroerer, W.; Muth, C.M.; Paulat, K.; Simon, P.; Heitkamp, H.-C.; Niess, A.; Tetzlaff, K. Hypoxia and cardiac arrhythmias in breath-hold divers during voluntary immersed breath-holds. Eur. J. Appl. Physiol. 2009, 105, 673–678.
- Brugger, ; Sumann, G.; Meister, R.; Adler-Kastner, L.; Mair, P.; Gunga, H.; Schobersberger, W.; Falk, M. Hypoxia and hypercapnia during respiration into an artificial air pocket in snow: Implications for avalanche survival. Resuscitation 2003, 58, 81–88.
- Strapazzon, ; Paal, P.; Schweizer, J.; Falk, M.; Reuter, B.; Schenk, K.; Gatterer, H.; Grasegger, K.; Dal Cappello, T.; Malacrida, S. Effects of snow properties on humans breathing into an artificial air pocket–an experimental field study. Sci. Rep. 2017, 7, 1–12.
- Strapazzon, ; Gatterer, H.; Falla, M.; Dal Cappello, T.; Malacrida, S.; Turner, R.; Schenk, K.; Paal, P.; Falk, M.; Schweizer, J.; et al. Hypoxia and hypercapnia effects on cerebral oxygen saturation in avalanche burial: A pilot human experimental study. Resuscitation 2021, 158, 175–182.
- Grissom, K.; Radwin, M.I.; Harmston, C.H.; Hirshberg, E.L.; Crowley, T.J. Respiration during snow burial using an artificial air pocket. JAMA 2000, 283, 2266–2271.
- Radwin, I.; Grissom, C.K.; Scholand, M.B.; Harmston, C.H. Normal oxygenation and ventilation during snow burial by the exclusion of exhaled carbon dioxide. Wilderness Environ. Med. 2001, 12, 256–262.
- McIntosh, E.; Little, C.E.; Seibert, T.D.; Polukoff, N.E.; Grissom, C.K. Avalanche airbag post-burial active deflation—The ability to create an air pocket to delay asphyxiation and prolong survival. Resuscitation 2020, 146, 155–160.
- Roubik, ; Sieger, L.; Sykora, K. Work of breathing into snow in the presence versus absence of an artificial air pocket affects hypoxia and hypercapnia of a victim covered with avalanche snow: A randomized double blind crossover study. PLoS ONE 2015, 10, e0144332.
- Wik, ; Brattebø, G.; Østerås, Ø.; Assmus, J.; Irusta, U.; Aramendi, E.; Mydske, S.; Skaalhegg, T.; Skaiaa, S.C.; Thomassen, Ø. Physiological effects of providing supplemental air for avalanche victims. A randomised trial, Resuscitation 2022, 172, 38–46.
- Roubik, ; Filip, J. Reliability and source of errors in end-tidal gas concentration evaluation algorithms during avalanche snow and rebreathing experiments. Lek. A Tech. Clin. Technol. 2017, 47, 73–80.
- Horakova, ; Roubik, K. Performance of Different Pulse Oximeters Can Affect the Duration of Field Breathing Experiments. In Proceedings of the 2019 E-Health and Bioengineering Conference (EHB), 2019; pp. 1–4.
- Horakova, ; Sykora, K.; Sieger, L.; Roubik, K. Breathing Experiments into the Simulated Avalanche Snow: Medical and Technical Issues of the Outdoor Breathing Trials. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering 2018, IFMBE Proceedings; Lhotska, L., Sukupova, L., Lacković, I., Ibbott, G., Eds.; Springer: Singapore, 2019; Volume 68/1, pp. 711–717.
- Trivedi, S.; Ghouri, A.F.; Shah, N.K.; Lai, E.; Barker, S.J. Pulse oximeter performance during desaturation and resaturation: A comparison of seven models. J. Clin. Anesth. 1997, 9, 184–188.
- Roubik, ; Sykora, K.; Sieger, L.; Ort, V.; Horakova, L.; Walzel, S. Perlite is a suitable model material for experiments investigating breathing in high density snow. Sci. Rep. 2022, 12, 2070.
- E. Company. Datex Ohmeda S/5 Compact Anesthesia Monitor. In Technical Reference Manual; Madison, MI, USA, 2006.
- GE Carescape Monitors B850 and B650 User’s Manual; Milwaukee: WI, USA, 2013.
- Edan M3B Vital Signs Monitor User Manual, version 1.6; EDAN Instruments: San Diego, CA, USA, 2012.
- Radical-7 Operator’s Manual; Masimo: Irvine, CA, USA, 2012.
- Model 2500 PalmSAT. In Operator’s Manual; Nonin Medical Inc.: Plymouth, MN, USA, 2014.
- Roubik, ; Walzel, S.; Horakova, L.; Refalo, A.; Sykora, K.; Ort, V.; Sieger, L. Materials suitable to simulate snow during breathing experiments for avalanche survival research. Lek. A Tech. Clin. Technol. 2020, 50, 32–39.
- Nitzan, ; Romem, A.; Koppel, R. Pulse oximetry: Fundamentals and technology update. Med. Devices 2014, 7, 231–239.
- International Organization for Medical Electrical Equipment—Part 2-61: Particular Requirements for Basic Safety and Essential Performance of Pulse Oximeter Equipment ISO 80601-2-61:2017; 2019.
- Vagedes, ; Bialkowski, A.; Wiechers, C.; Poets, C.F.; Dietz, K. A conversion formula for comparing pulse oximeter desaturation rates obtained with different averaging times. PLoS ONE 2014, 9, e87280.
- McClure, ; Jang, S.Y.; Fairchild, K. Alarms, oxygen saturations, and SpO2 averaging time in the NICU. J. Neonatal. Perinat. Med. 2016, 9, 357–362.
- Goldman, M.; Petterson, M.T.; Kopotic, R.J.; Barker, S.J. Masimo signal extraction pulse oximetry. J. Clin. Monit. Comput. 2000, 16, 475–483.
- Jubran, Pulse oximetry. Crit. Care 2015, 19, 272.
- Horakova, ; Kudrna, P.; Roubik, K. Dynamic changes of perfusion index during hypoxemia and hypercapnia in outdoor experiments. In 2021 International Conference on e-Health and Bioengineering (EHB); IEEE: Piscataway, NJ, USA, 2021; pp. 1–6.
- Lawless, T. Crying wolf: False alarms in a pediatric intensive care unit. Crit. Care Med. 1994, 22, 981–985.
- Chambrin, -C.; Ravaux, P.; Calvelo-Aros, D.; Jaborska, A.; Chopin, C.; Boniface, B. Multicentric study of monitoring alarms in the adult intensive care unit (ICU): A descriptive analysis. Intensive Care Med. 1999, 25, 1360–1366.
- Taylor, ; Whitwam, J. The accuracy of pulse oximeters: A comparative clinical evaluation of five pulse oximeters. Anaesthesia 1988, 43, 229–232.
- Barker, J. “Motion-resistant” pulse oximetry: A comparison of new and old models. Anesth. Analg. 2002, 95, 967–972.
- Robertson, A.; Hoffman, G.M. Clinical evaluation of the effects of signal integrity and saturation on data availability and accuracy of Masimo SET® and Nellcor N-395 oximeters in children. Anesth. Analg. 2004, 98, 617–622.
- Van de Louw, ; Cracco, C.; Cerf, C.; Harf, A.; Duvaldestin, P.; Lemaire, F.; Brochard, L. Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med. 2001, 27, 1606–1613.
- Nitzan, ; Nitzan, I.; Arieli, Y. The Various Oximetric Techniques Used for the Evaluation of Blood Oxygenation. Sensors 2020, 20, 4844.
- Jubran, Pulse oximetry. In Principles and Practice of Intensive Care Monitoring; Tobin, M.J., Eds.; McGraw-Hill: New York, NY, USA, 1998; pp. 261–289.
- Johnston, D.; Boyle, B.; Juszczak, E.; King, A.; Brocklehurst, P.; Stenson, B.J. Oxygen targeting in preterm infants using the Masimo SET Radical pulse oximeter. Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F429–F433.
- Ross, A.; Newth, C.J.; Khemani, R.G. Accuracy of pulse oximetry in children. Pediatrics 2014, 133, 22–29.
- Bachman, E.; Newth, C.J.; Ross, P.A.; Iyer, N.P.; Khemani, R.G. Characterization of the bias between oxygen saturation measured by pulse oximetry and calculated by an arterial blood gas analyzer in critically ill neonates. Lek. A Tech. Clin. Technol. 2017, 47, 130–134.
- Ikeda, ; MacLeod, D.B.; Grocott, H.P.; Moretti, E.W.; Ames, W.; Vacchiano, C. The accuracy of a near-infrared spectroscopy cerebral oximetry device and its potential value for estimating jugular venous oxygen saturation. Anesth. Analg. 2014, 119, 1381–1392.
- Strapazzon, G.; Gatterer, H.; Falla, M.; Cappello, T.D.; Malacrida, S.; Turner, R.; Schenk, K.; Paal, P.; Falk, M.; Schweizer, J.; et al. Hypoxia and hypercapnia effects on cerebral oxygen saturation in avalanche burial: A pilot human experimental Resuscitation 2020, 158, 175–182.
- Gehring, H.; Hornberger, C.; Hornberger, H.; Schmucker, The effects of motion artifact and low perfusion on the performance of a new generation of pulse oximeters in volunteers undergoing hypoxemia. Respir. Care 2002, 47, 48–60.
- Yamaya, ; Bogaard, H.J.; Wagner, P.D.; Niizeki, K.; Hopkins, S.R. Validity of pulse oximetry during maximal exercise in normoxia, hypoxia, and hyperoxia. J. Appl. Physiol. 2002, 92, 162–168.
- Ricart, A.; Pages, T.; Viscor, G.; Leal, C.; Ventura, J.L. Sex-linked differences in pulse oxymetry. Br. J. Sports Med. 2008, 42, 620–621.
